
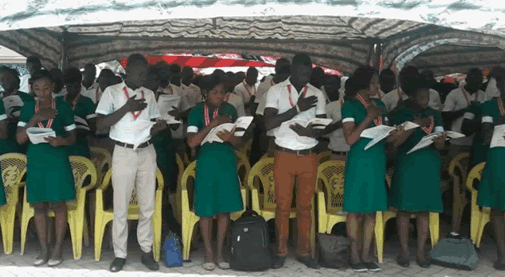
The Teachers and Educational Workers’ Union (TEWU) of Trade Union Congress (TUC) Ghana has suspended its industrial action, declared on November 18, 2024.
The post TEWU-TUC-Ghana suspends industrial action, resumes work on November 25 appeared first on Ghana Business News.
]]>
 The Teachers and Educational Workers’ Union (TEWU) of Trade Union Congress (TUC) Ghana has suspended its industrial action, declared on November 18, 2024.
The Teachers and Educational Workers’ Union (TEWU) of Trade Union Congress (TUC) Ghana has suspended its industrial action, declared on November 18, 2024.
The Union urged its members to resume full work by Monday, November 25, 2024.
King James Azortibah, the General Secretary of the Union, announced this in a statement copied to the Ghana News Agency in Accra.
“We assure our cherished members that the leadership of TEWU of TUC-Ghana is bent on ensuring that there will be finality to the issue of the conditions of service of the affected institutions for immediate implementation.
“Our members are being shortchanged with the continuous delay in concluding and implementing the Conditions of Service, and this cannot be allowed to continue,” the statement said.
TEWU of TUC-Ghana on Monday, November 18, 2024, embarked on an indefinite industrial action, over more than four years delay in concluding and implementing the Conditions of Service for its member institutions.
The institutions are the Ghana Education Service, the Ghana Museums and Monuments Board, the Ghana Library Authority, and the Public and Technical Universities.
The National Labour Commission on Wednesday, November 20, 2024, issued a directive that the strike should be called off while the Union and its various managements concerned report back on Wednesday, November 27, 2024, for the Commission to hear the substantive case.
Source: GNA
The post TEWU-TUC-Ghana suspends industrial action, resumes work on November 25 appeared first on Ghana Business News.
]]>
In Laura Ingalls Wilder’s view “the real things haven’t changed. It is still best, to be honest, and truthful; to make the most of what we have; to be happy with simple pleasures, and have courage when things go wrong.” There is a narrative around health information especially health inputs and how politicians spin these […]
The post Spin on health numbers: This call for equity must be backed by plans and deeds appeared first on Ghana Business News.
]]>
 In Laura Ingalls Wilder’s view “the real things haven’t changed. It is still best, to be honest, and truthful; to make the most of what we have; to be happy with simple pleasures, and have courage when things go wrong.”
In Laura Ingalls Wilder’s view “the real things haven’t changed. It is still best, to be honest, and truthful; to make the most of what we have; to be happy with simple pleasures, and have courage when things go wrong.”
There is a narrative around health information especially health inputs and how politicians spin these numbers. I can always live with the mischief but when citizens buy into this narrative and swallow the information hook, line and sinker I get worried. I have on occasion pointed out that we need to be honest about our health human resource numbers to inform honest conversations around what our resource gaps look like. This could also aid us to think out of the box in a way that may facilitate the conversion of one health human resource into another to correct disparities.
Last week, it was reported that 495 Emergency Medical Technicians (EMTs) of the National Ambulance Service (NAS) had passed out at the Paramedic and Emergency Care Training School at Nkenkasu in the Ashanti Region. This number increased the total number of EMTs to 2,154 across the country. Meaning our current Paramedic to population ratio is 0.072 paramedics to 1000 population. This number also equates to 7.8 paramedics per each constituency assuming the spread of this vital health human resource was equitable across the country.
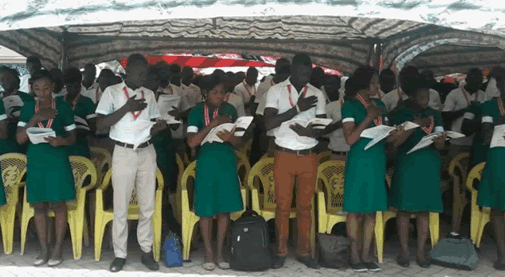
In that same week, 8,610 nurses, nurse assistants and midwives from the southern zone of Ghana were inducted into the profession having passed their professional licensing examination. A simple look at this number should set readers thinking. As this gives an idea of the total number of nursing human resources that are trained and licensed in the country annually.
The journeys of these two groups of vital health human resources in the coming weeks, months and years would be very contrasting. Whilst the paramedics enter the job market with employment certainty, the same cannot be said for their nursing colleagues. Even though our nurse to population ratio currently is 1.2 nurses to 1000 population. The reason being thanks to financial constraints the government cannot absorb all these nurses into the health sector. Meaning almost all of them are likely to join the backlog of unemployed nursing professionals. A situation that we must not countenance.
I will propose we aim at 0.5 paramedics per 1000 population or a total of 15,000 paramedics for the entire population.
At the induction of the nursing professionals, Health Minister Kwaku Agyeman-Manu urged stakeholders in healthcare delivery to help achieve universal access to improved health services nationwide. My view is that his ministry can show leadership by first ensuring that the disparity in the paramedic to population ratio is address as a matter of urgency. To do this will require a clear strategy with an ideal ratio to get to and in what period. I will propose we aim at 0.5 paramedics per 1000 population or a total of 15,000 paramedics for the entire population.
Carefully looking at this number, the first realisation will be that our paramedic deficit based on current numbers will be 12,846. Which indicates that with only one Emergency Medical Technician training school turning out approximately 500 students annually it will take us about twenty-five years to realise this goal. A situation we cannot accept. Considering that we have many nursing schools and have a backlog unemployed, my first suggestion will be to approach this skilled health labour pool to ascertain how many of them will be willing to divert and undertake directed training to become paramedics. My view is that with their job prospects low, many may take up this offer. These can then be taken through a crash course and certified.
The capabilities of nurses in emergency care even without specific training in this area cannot be underestimated. This was brought into the spotlight when at the same function, Samira Bawumia succumbed to the realities of heat exhaustion. Her praise for the professionalism of the nurses around in managing her condition attests to this fact.
My second suggestion will be to find a way of allowing trainee nursing students to obtain essential skills in emergency medicine whilst at school on an optional basis. Apart from the fact that this could improve their employment prospects and career pathways, it could also provide a quick route to bridging the nation’s paramedic deficit.
More importantly, it could also serve as a feeder route for the training of emergency care nurses for many districts that lack this nursing skill mix in their accident and emergency departments. Priority could even be given to trainees who opt to go to more deprived parts of the country or are in nursing training institutions in those areas as a means of circumventing the age-old barriers that prevent health professionals from taking up job opportunities in these parts of the country. This training option could then be reviewed after a period of say five years or even less depending on how quickly our paramedic deficit is fixed.
My second suggestion will be to find a way of allowing trainee nursing students to obtain essential skills in emergency medicine whilst at school on an optional basis.
Mr Minister, it will be much easier to attract stakeholders into the more deprived areas to ensure improved health access if your establishment is seen to be proactively helping to bridge not only the health human resource deficits but also the disparities that exist as well as the spread of these human resources across the country.
It will be diabolical if in the wake of purchasing new ambulances and equipping the Ghana Ambulance Service with pickup vehicles we fail to ensure that the use of these infrastructures is optimised. It thus cannot be accepted if emergency services were not available to a citizen on the account that though there were ambulances, there were no paramedics to operationalise them.
I would conclude by stating that if in the abundance of nurses, we cannot make the most of what we have and convert some into paramedics to fix our deficit, we would have failed to make the most of what we have and our innate ability to think outside the box.
By Kwame Sarpong Asiedu
The post Spin on health numbers: This call for equity must be backed by plans and deeds appeared first on Ghana Business News.
]]>
“When we least expect it, life sets us a challenge to test our courage and willingness to change; at such a moment, there is no point in pretending that nothing has happened or in saying that we are not yet ready. The challenge will not wait. Life does not look back. A week is more […]
The post A leadership dilemma: Maintaining the status quo or to cross the Rubicon appeared first on Ghana Business News.
]]>
“When we least expect it, life sets us a challenge to test our courage and willingness to change; at such a moment, there is no point in pretending that nothing has happened or in saying that we are not yet ready. The challenge will not wait. Life does not look back. A week is more than enough time for us to decide whether or not to accept our destiny.”
The Ghana Health Service (GHS) has a new Director-General following the exit of Dr Anthony Nsiah Asare on November 1. I will leave a verdict on his stewardship for another day, preferring instead to look at what this crossroads brings.
I have never been a fan of how chief executives of important state institutions like the GHS are appointed at the discretion of the President and would rather prefer a competitive process using a search party. I have also wondered whether this role should continue to be the preserve of medical doctors and if so why?
My preference is as a result of the fact that in a competitive process clear visions of the applicants can be contrasted and the most appropriate candidate appointed. In the area of health, this allows the candidates understanding of the new frontiers of medicine to be explored as well as how they could leverage this to improve the fortunes of Ghana’s health delivery system. This will also allow those without a medical background but with a good understanding of healthcare to pitch their ideas and experience. Such opportunities have been given in many countries with brilliant results. For example, the current Chief Executive of the United Kingdom’s National Health Service Simon Stevens is a non-medic health manager with a wide range of experience in health delivery across the globe.
Secondly, the search party knowing the challenges in our health sector could have performance benchmarks that could be part of any service contract the appointee is given. These can then be used as a means of accessing performance periodically. It could also aid the appointing authority to make informed decisions as to whether the continuous stay of any appointee in office was beneficial or counterproductive. Finally, this could be the beginning of tenured rather than politically tied leadership and allow the Director-General the space to plan at least in the short and medium-term.
Unfortunately, the reality is we are a distance away from this form of openness mainly due to our winner takes all brand of democracy and must make the best out of our current circumstances.
Since it was announced that Dr Baffuor Awuah former Medical Director of Komfo Anokye Teaching Hospital will take over in an acting capacity, I have been wondering what this will bring to the quality of health that institutions under the GHS deliver. I have because many have argued that in most things’ leadership is the key and catalytic cause and that all other deliverables are a direct effect of this catalyst. I have also looked at how much time he has to make an impact knowing well that our next electoral cycle occurs in thirteen months and that he could be out of this job should the electoral fortunes of his appointing authority take a nosedive.
The new Director-General takes over at a time when Ghana has been sliding down in the world rankings of life expectancy and many of the other health outcome indicators. Childhood immunisation coverage is also on the decline with the percentage of eligible children immunised against measles by age two dropping to 92 per cent and diphtheria, pertussis (or whooping cough), and tetanus (DPT) down to 96 per cent all from a 99 per cent coverage just over two years ago. Geriatric care improvements have been abysmal over the years with the percentage of the population living above the age of sixty- five dropping marginally from a high of 3.5 per cent in 2010 to the current 3.38 per cent, whilst those over the age of seventy accounts for only 1.81 per cent of our population. Reports of poor-quality health service delivery across all ages are rife and health human resource numbers nothing to be pleased with.
On the surface, one would wonder why any sane human would want to accept this otherwise poisoned chalice? However, I strongly believe that he has a very good chance of making a mark and excelling in this new role as long as he realises the gravity of the task ahead. To start with he would have to work with virtually the same team he is inheriting and would need to find novel ways of understanding what their challenges are. He will then have to outline his vision and show how he wants to see this implemented.
In doing so, I hope he would have extensive discussions with ordinary Ghanaians as a means of understanding their views on the performance of the institution he is taking over. If he did, he would realise that the confidence citizens have in our health delivery system is very low. He would also hear horrifying stories of why this is the case. My advice to him is that he should not get defensive but rather take all this feedback in good stride. After all, he is here to make a mark and not to deliver business as usual.
In the end, he would have to make a judgement whether the health delivery model, especially in the area of primary health, is fit for purpose? He would then have to decide based on his answer to this question whether to stay the current course or to change direction. If he decides to stay the course, he should find little resistance from the team he is inheriting and would be easily accepted. If he chooses to opt for an alternative approach, he should realise that the fear of change will be his biggest headache.
Either way, he should remember this is his date with destiny, one that will put his courage to the ultimate test and know that his legacy will be defined by the choices he makes especially in the first three months of his stewardship. I hope he makes the right choices that will result in significant unlearning and relearning. Having said that I wish him well for it is in the entire national interest that he gets this one right.
By Kwame Sarpong Asiedu
The post A leadership dilemma: Maintaining the status quo or to cross the Rubicon appeared first on Ghana Business News.
]]>
Tiffanie DeBartolo in How to Kill a Rock Star had this to say. “Did you really want to die? No one commits suicide because they want to die. Then why do they do it? Because they want to stop the pain.” Sometime in 1994, whilst in my undergraduate years, I received a phone call from […]
The post How is suicide a crime? appeared first on Ghana Business News.
]]>
 Tiffanie DeBartolo in How to Kill a Rock Star had this to say. “Did you really want to die? No one commits suicide because they want to die. Then why do they do it? Because they want to stop the pain.”
Tiffanie DeBartolo in How to Kill a Rock Star had this to say. “Did you really want to die? No one commits suicide because they want to die. Then why do they do it? Because they want to stop the pain.”
Sometime in 1994, whilst in my undergraduate years, I received a phone call from my father late in the night the content of which I will never forget. His request was for me to come to pick him up as the police had attended our home on KNUST campus. With a mixture of anxiety and apprehension, I drove from the University Hall and got home to the news that one of his staff who had just returned from studying abroad had been found dead in his hotel room. Together we drove to the hotel, the scene that greeted me is one I can never erase from my memory. On the floor in a pool of white foaming vomit lay a man I knew very well. Next to him was a glass and some leftover tablets. He was a biochemist and had thought this one through.
The policemen took statements from the hotel staff and arranged the evacuation of his mortal remains to the mortuary. He had no immediate family close by so the onus fell on my father to inform his family in the morning. When this happened, there was the shock and wailing that accompanies sudden death. Out of the blue, an elderly man rebuked those in grief, claiming the deceased was selfish and had taken the easy way out. Even amongst the intellectual fraternity within the university, he was deemed a coward. I questioned my Dad on his views about the incident, this was what he had to say. “Suicide is neither an easy option or an act of cowardice. It is rather a reaction to an incident that can often be traced to a mental imbalance either chronic or transient. I advise that you read about it rather than form your views based on societal norms.”
This was the beginning of my journey into understanding one of the most stigmatised life endings in our society. Since the year 2000, suicide rates in Ghana has been increasing. From a figure of 4.30 deaths per 100,000 citizens, it had increased by 23.25% to 5.30 per 100,000 in 2016 and increased further by 9.4% to 5.8 per 100,000 by the end of 2018. Meaning in 2018, 1,740 Ghanaians took their own lives. The prevalence of this phenomenon is highest amongst males with 9.1 males in 100,000 choosing this option compared with 2.1 females in 100,000. This trend is in line with the suicide rate gender split found in most developed countries.
It is known that three times more people attempt suicide than those who succeed and that even more contemplate this act but never carry it out. I leave readers to work out on this basis how many people who potentially could have been incarcerated under our penal code for an act that should never pass as a crime.
Suicidal behaviours are complex and not easily explained. Several factors ranging from social, psychological, and cultural singularly or through intrinsic interactions lead a person to suicidal thoughts or behaviour. Thus, often the final act is after considerable thought but on occasion can be impulsive too. The main determinants of whether one with suicidal thoughts will actually carry these through are their ability to access help in a timely manner, coupled with the level of support they receive during the period as well as the level of media reportage that suicides receive and the extent to which the mental health, substance abuse and suicidal ideation are stigmatised.
It is known that three times more people attempt suicide than those who succeed and that even more contemplate this act but never carry it out.
In a country where mental health and all its associations are ill funded and the stigma is huge, it is therefore incredulous that rather than work to improve the situation, many still believe that this act is in the least demonic and at worst criminal. Can it not be argued that if there is any criminality at play it’s the state and those who fan the flame of mental health stigma who are the real criminals? Can actions that put barriers in the way of those who need help thus driving them to the point of suicide not be tantamount to manslaughter? If these are to be argued then is the above not enough reason that this aspect of our criminal code has outlived its usefulness?
Why then can a Deputy Speaker of Ghana’s Parliament argue that, since nobody has ever been prosecuted in the country for attempting to commit suicide, the demands for a change in the law are needless? Does he not realise that the very existence of that law ensures that many who contemplate suicide do not seek help and strive to succeed? Is that in itself not compounding a problem that is on the rise? Is he not aware that in a country where poverty is rife and the gap between the haves and have nots is widening the pressures on both in a society increases the propensity for suicidal thoughts to manifest?
Even more worrying is the view of the Minority Leader Haruna Iddrisu who argues that the status quo be maintained. Hear him, “I disagree that we should decriminalise suicide. Unacceptable behaviour must be punished and deterred, you don’t want a society where you encourage young children that if they have a problem, they can kill themselves. Which society develops that way?” Does the medical evidence support his view that suicide is unacceptable behaviour? Has he bothered to acquaint himself with the drivers that contribute to suicide?
The young academic who passed away on that fateful night had just completed his PhD. He had a lot of life ahead of him and the potential to contribute through intellectual knowledge transfer, research, taxes and the training of other academics to the development of Ghana.
Many in our legislature backing the trend of the general population are unschooled about matters relating to mental health and need to urgently unlearn this foul narrative. In doing so, they must understand that on the contrary societies that are developing at tremendous pace are doing this thanks to many of their leading brains in academia, politics, business, medical and legal fraternities who have been suicidal themselves but found help, were not stigmatised, were giving a way out and are now returning the favour through their positive contributions they make to their country’s economies.
The young academic who passed away on that fateful night had just completed his PhD. He had a lot of life ahead of him and the potential to contribute through intellectual knowledge transfer, research, taxes and the training of other academics to the development of Ghana. Sadly, we lost this contribution because he didn’t seek help or if he did could not access it for some of the reasons I earlier enumerated. I owe it to his memory and to the memory of many others who have passed away to speak up against the near tyranny that some in our legislative house may be engaging in as far as the decriminalisation of suicide is concerned.
Those who commit or contemplate suicide are not criminals, neither do they want to die. By all indications, they choose this option because they want to end their pain whether real or imaginary. It is our responsibility to help assuage their pain. As the nation undergoes further development, we cannot help but accept that if we do not change our perceptions around mental health in general and suicide, in particular, we would soon become yesterday’s country in tomorrow’s world.
By Kwame Sarpong Asiedu
The post How is suicide a crime? appeared first on Ghana Business News.
]]>
“Perhaps this is what the stories meant when they called somebody heartsick. Your heart and your stomach and your whole insides felt empty and hollow and aching.” Gabriel García Márquez Bereavement is not a pleasant experience. Anyone who has suffered the loss of a loved one will attest to this. In the last week, I […]
The post Need to move a step further with breast cancer awareness in Ghana appeared first on Ghana Business News.
]]>
“Perhaps this is what the stories meant when they called somebody heartsick. Your heart and your stomach and your whole insides felt empty and hollow and aching.” Gabriel García Márquez
Bereavement is not a pleasant experience. Anyone who has suffered the loss of a loved one will attest to this. In the last week, I have seen posts made by many close friends who have lost close family and acquaintances. As I express my condolences on each occasion, I have also paused to look at the ages at which these unfortunate deaths are occurring. In recent times, I have come to believe that any loss of life that occurs in Ghana before age 63.5 years is avoidable and must give cause for concern.
With this age being our average life expectancy, I cringe when I read the phrase “Rest in Peace” on many of these obituaries. I do because as a health professional who has occasioned to be at the bedside of dying patients, I have seen what it means to pass away in peace and what it means to depart this earth in anguish. Any health professional can tell you the anguish with which patients speak about their children, family and spouses in the final moments before their life is cut short prematurely in their prime. In a world full of cruelty, many are even unsure how the future of their children is going to turn out. If anything, I am inclined to believe in the cliché that many turn in their graves.
What even gets to me is the fact that we have all become accepting of these happenings, throwing up our hands as though we are hapless. The truth is we are not. Currently, health is progressing at a pace where many of these deaths can be predicted and avoided. Having lost my mother to endometrial cancer back in 2015 and knowing that many cancers are genetically modulated, I have always been an advocate for early screening. Sadly, many of us place little value on the information inherently stored in our genes.
Every October, I am gratified at the level of awareness breast screening is giving all be it under the pretext of “freeing the tatas.” However, I cannot help but wonder if we would not be better off getting our women to test for mutations of BRCA1 and BRCA2 human genes, the best predictors currently of female breast and ovarian cancers. Especially when these genes have also been associated with increased risks of several additional types of cancer. Would it not be better knowing the risk even before a lump however small appeared in the breast?
Let’s look at the statistics on breast cancer for a while. Data available from the United States National Cancer Institute and corroborated by other cancer centres indicates that “about 12 per cent of women in the general population will develop breast cancer some time during their lives.”
A recent large study published by Kuchenbaecker and associates in the Journal of the American Medical Association (JAMA) estimated that about 72 per cent of women who inherit a harmful BRCA1 mutation and about 69 per cent of women who inherit a harmful BRCA2 mutation will develop breast cancer by the age of 80. Is this not enough reason to push for genetic screening?
On May 14, 2013 Angelina Jolie in an article in the New York Times decided to open up on her decision to have a preventive double mastectomy. She explained that her mother fought cancer for almost a decade and died at 56. “She held out long enough to meet the first of her grandchildren and to hold them in her arms,” she said. But my other children will never have the chance to know her and experience how loving and gracious she was. Before then Jolie had lost her grandmother to the same disease.
Reading the article again this morning, I could feel the anguish in her words and roundly understood why she opted to undergo testing for these mutant genes and acted the minute she was found to be a carrier of these mutations. But what got me thinking was her decision to go public with such a deeply personal story. Suddenly, it all made sense. She was not prepared to take chances with her life and miss out on family moments as her mother and grandma had. She also knew that with her status, speaking up was a way to empower many women without a voice. She was thus prepared to put her head above the parapet so that neither she nor those willing to read and take heed will have the phrase “Rest in Peace” on their obituary earlier than it was otherwise necessary.
The real challenge in going down this route of pre-emptive testing for Ghana would be education. In a country where post-mortems are frowned upon by many and little value is put on their importance by families, convincing the majority to test for a gene especially when there is no sign of ill health will be a tall order. Should they even agree to test, having the result with no obvious signs of disease will lead many to procrastinate. Then there is the issue of cost and who should be paying for these tests based on the low spending ability of many Ghanaians. Much as these are real obstacles, I am one who believes when there is the will there is always a way.
My belief that this can be done is not without basis though. I listened to a podcast on BBC that indicated that a start-up 54gene led by Abasi Ene-Obong identifying that only about two per cent of genomics research worldwide has been undertaken on African subjects and the serious disadvantage this puts us all at, they have set out to build the largest collection of African DNA. This for me is the beginning of the process of availing Africans to the potential that lies untapped in genetics. Ambitions like this for me are worthy and I just hope others will jump on board.
We cannot continue to see people feel heartsick and empty in a world where knowledge in health is expanding exponentially and expect that they rest in peace. To do so will be to betray our intelligence and to let down many loved ones. Just so you know, when my mum passed, I advised all females in my matrilineal line to get screened for Braca1 and Braca2. It was the least I could do to assuage their pain.
By Kwame Sarpong Asiedu
The post Need to move a step further with breast cancer awareness in Ghana appeared first on Ghana Business News.
]]>
Christophe Galfard in his book The Universe in Your Hand argues that “a clock that is moving through space at a very fast speed does not tick at the same rate as a slow-moving watch gently attached to your wrist as you stroll on a tropical beach. The idea of a universal time – a […]
The post The Ghana health debate: going in cycles appeared first on Ghana Business News.
]]>
 Christophe Galfard in his book The Universe in Your Hand argues that “a clock that is moving through space at a very fast speed does not tick at the same rate as a slow-moving watch gently attached to your wrist as you stroll on a tropical beach. The idea of a universal time – a godlike clock that could somehow sit outside our universe and measure, in one go, the movement of everything in it, how its evolution unfolds, how old it is and all that – does not exist.”
Christophe Galfard in his book The Universe in Your Hand argues that “a clock that is moving through space at a very fast speed does not tick at the same rate as a slow-moving watch gently attached to your wrist as you stroll on a tropical beach. The idea of a universal time – a godlike clock that could somehow sit outside our universe and measure, in one go, the movement of everything in it, how its evolution unfolds, how old it is and all that – does not exist.”
Being very interested in sports I tend to agree with him. Measurement of anything in absolute numbers has very little relevance. Thus, in professional football, for example, teams are relegated because although they may win several games over a season, others win a lot more and surpass them. Sadly, in Ghana’s health sector we seem to enjoy discussions in absolute numbers, treating the country as an isolate.
It is not uncommon therefore to find a discussion around say health worker recruitment numbers being had based on which political party employed more while in government compared with the other. I have over the years followed some of these debates in complete surprise as to what if any the value addition is. In doing so I have wondered if there is any benchmarking when having these debates?
Let me use the number of doctors in our country for an illustration. The country as at the end of 2017 had 4,016 doctors according to data from the Ghana Health Service with a doctor to population ratio of 0.2: 1,000. However, the optimum doctor to population ratio that the World Health Organisation recommends is 1: 1000. Meaning, the country with a population of 29.2 million in that year required about 29,200 doctors. A look at the total number of doctors by year-end 2016 will show that there were 3,365. On the surface, it is easy for the current government to argue that they added approximately 700 more which was higher than any year since 2008.
But, in reality, this must not be a cause for celebration. It is not because, with a population growth rate of 2.25 per cent and approximately a net number of 700,000 citizens being added to our population annually, the requirements for doctors is also increasing at 700 each year. The result being that this level of recruitment is not even good enough or at best breaks even in catering for the medical human resource needs due to population expansion, let alone attempt to make a dent in the deficit we already have.
This illustration has led me to wonder how citizens have allowed this debate to fester all this while without any concerted challenge to this otherwise warped and baseless self-aggrandisement? As if that is not bad enough, we carry this into our technocratic discussions around many health-related indicators. It is as though Ghana is an island and our health outcomes stand in isolation. Let’s just look at a couple of these indicators.
In 2018, Ghana’s infant mortality rate was 34.9 deaths per thousand live births. Infant mortality has fallen from 120.5 deaths per thousand live births in 1969 to the current figure in 2018. A four-fold decrease over five decades to 3.49 per cent. Looking at it as a standalone value, again it’s easy to celebrate. But in comparison not so much so. Rwanda in 1969 had an infant mortality rate of 129.1 deaths per thousand births rising to 148 deaths per 1000 in 1977 at a time when Ghana’s rate was is in steady decline. In 1994 the figure for that country was 125.80 deaths per thousand births. Currently, Rwanda has an infant mortality rate of 17 deaths per thousand births or 1.7 per cent (50 per cent) less than Ghana’s death rate.
The result of this is that Ghana is the 45th country in which a mother is likely to lose their child at birth or within the first year of life amongst 193 countries ranked by the WHO whilst Rwanda is fourteen places better at 59th. Having dropped three places since the turn of the millennium. With Kenya, Senegal and Malawi all passing us by.
Another indicator I will want to look at is female life expectancy. In 2017, female life expectancy for Ghana was 64.5 years. Having increased from 49.4 years in 1968, growing at an average annual rate of 0.55 per cent. On the other hand, female life expectancy for Liberia was 64.7 years in the same year passing Ghana in the world rankings from the previous year. Their longevity increased from 40.3 years (9.1 years lower than Ghana) in 1968, growing at an average annual rate of 0.97 per cent (just under twice the growth rate of Ghana over the same period). This was in spite of them fighting two civil wars between 1989 and 2003. Here too, Ghana dropped eleven places from 153 in the year 2000 to 164 in 2017. Having been bypassed by countries like Rwanda, Liberia, Eritrea, Ethiopia and Sudan just to name a few. Should society and mothers especially be proud of our backward slide? In my view, hell no.
It is safe to say from the above that though Ghana has been making advances in many of its health indicators, other countries are doing a lot better. To use the analogy of football again, if Ghana was in the first division in 1970 for many of our health indicators, we would have been relegated to division three though we have won a few matches along the way. This is why I insist that how we have our debates in health comparing one set of mediocre outcomes to another and thumping our chests in the process is flawed. We need to accept that Ghana is not an island but a country that once prided itself as the star of Africa. A star which based on some of these performances is dimming rapidly.
I will conclude by saying the only reason why our governments have gotten away with this till date is because as citizens, we have failed to depoliticise our health outcomes and have turned it into a turf ground where political opportunists play Russian roulette with our ignorance, health and quality of life. The only way we can reverse this is to make ourselves conversant with comparative data especially for countries that are achieving better outcomes whilst spending less money per citizen in the health sector.
Just to put some financial context on these outcomes, all countries mention in this text have spent less per citizen on health compared with Ghana since the year 2000. With Rwanda which has consistently spent the least achieving the most impressive outcomes. As of 2017, the health expenditure per capita of that country was $48.08 with Ghana and Liberia at $68.31 and Kenya $66.21. We have been strolling on a tropical beach with much to spend but little to show.
By Kwame Sarpong Aisedu
The post The Ghana health debate: going in cycles appeared first on Ghana Business News.
]]>
“Simple can be harder than complex: You have to work hard to get your thinking clean to make it simple. But it’s worth it in the end because once you get there, you can move mountains.” Steve Jobs This week, the Deputy Minister of Health Tina Mensah announced that the five-year bonding of nurses trained […]
The post When the numbers confront the rhetoric in Ghana’s management of nurses appeared first on Ghana Business News.
]]>
“Simple can be harder than complex: You have to work hard to get your thinking clean to make it simple. But it’s worth it in the end because once you get there, you can move mountains.” Steve Jobs
This week, the Deputy Minister of Health Tina Mensah announced that the five-year bonding of nurses trained in public health institutions had been scrapped. This decision comes on the back of government struggling to employ nurses though Ghana has a nursing deficit. Bonding of nurses was introduced by the government of J.A. Kufuor in 2005 as a means of curbing nursing and midwife brain drain that was impacting negatively on healthcare delivery. At that time, most nurses were promptly absorbed into our health system following graduation, a situation that does not exist today. Therefore, on the surface, this decision must be welcomed as it allows these nurses to seek employment elsewhere. However, it still opens up the debate on our health strategy and policy planning.
To start with, Ghana’s healthcare expenditure is under considerable strain. According to data from the Ministry of Health, Ghana’s health expenditure per capita (the average amount spent by the government on each citizen in the area of health) is $68, having peaked in 2013 at $111. Of this close to 60% is spent on the payment of salaries of health sector human resources. Meaning government has very little room to manoeuvre when it comes to increasing human resource numbers. With other countries clamouring for our nurses’ thanks to degree equivalence especially in Commonwealth countries, it is only sensible that these nurses are freed so they can earn a living.
The irony, however, is that though they are being allowed to leverage their qualifications elsewhere, the government has been silent on the allowances we pay to these nurses. It should not take a rocket scientist to work out that unless a means is found to recoup value from these nurses wherever they find themselves this stipend would soon become an unnecessary drain on the already stretched finances of the health sector. It could even be argued that we may by default be funding the health systems of countries otherwise wealthier than we are. I will seek to explain.
Take the United Kingdom as an example, data from the think tank King’s Fund, suggests there more than 30,000 extra nurses are required currently with the number expected to increase to 70,000 within five years. With the cost of £70,000 to train a nurse from scratch, it is now widely accepted that the country cannot meet its training requirements in the short to medium term. Even then and with the shortage of nurses estimated to have cost the National Health Service (NHS) about £2.4 billion in 2018, trainee nurses are still expected to pay fees. Though they are eligible to apply for a bursary from the NHS, a reduced maintenance loan from Student Finance England and a £1000 grant, these funds are based on an eligibility criterion that relies on household income. This can be your income, your parents’ income, or that of your partner, spouse or civil partner.
With this in mind, a nurse trained in Ghana with state handouts who migrate to the UK is at a considerable advantage as they are devoid of any student loans. Will this advantage not lead to a situation where Ghana becomes a training ground for nurses who simply need to pass an English language exam and prove equivalence based on a computer-based test and practical skills assessment? If that is the case then by extension will Ghanaian public funds not simply be paying for better healthcare in England?
It even looks more diabolical when one realises that the United Kingdom has a health expenditure per capita of $3,958 (approximately sixty times that of Ghana) and a current nurse to population ratio of 8.3 to 1000 with Ghana having 1.2 to 1000 population (a difference of seven nurses for every 1000 citizens).
I understand the political ramifications of any conversations around trainee nursing allowances. However, I struggle to make sense out of how as a people we can continue to fund this in the light of our inability to employ this vital health human resource. My views on Ghana’s nursing deficit and how we seem clueless about managing it are well known. However, I believe that the time has come for us to peel off our political cloaks to have an honest conversation. A conversation that looks holistically at our current nursing numbers, what our nursing requirements are going to be in the next decade, whether we genuinely want to bridge our nursing deficit and as to whether politics rather than technocratic planning should dictate our nursing recruitment and training strategy.
It even looks more diabolical when one realises that the United Kingdom has a health expenditure per capita of $3958 (approximately sixty times that of Ghana) and a current nurse to population ratio of 8.3 to 1000 with Ghana having 1.2 to 1000 population (a difference of seven nurses for every 1000 citizens).
It is not surprising that the government gave no reasons for its decision to moving away from the bonding of nurses. On the contrary, I am surprised that the announcement did not receive any scrutiny but passed more or less with a whimper. I am because by all indications, nurses are the face of healthcare provision in Ghana and the health professionals many of us come into routine contact with when we experience episodes of ill health.
We often complain when in our view the level of care they provide is below par. Yet, seem indifferent when decisions that affect their numbers and resourcing are taken. The truth is we cannot be this apathetic at best and extremely partisan at worst in these matters and expect improvement in the quality of healthcare we receive or our health outcomes. Our nurse to population ratio has been dropping since 2013 when it was 1.59 nurses to 1000 citizens to our current 1.2 to 1000. Yet, we are told that more nurses have been employed in the last two years than in any other year in recent times. How we have failed to peruse the numbers and challenge these assertions defies me.
The irony is that the government may be right on their nursing recruitment claim but that may just be a smokescreen. This is because, with a population growth rate of 2.2 per cent annually, approximately 3.8 million people have been added to Ghana’s population of 26,607,642 since 2013 meaning just to account for population growth 3,800 extra nurses (634 annually) would have had to be recruited just to keep our nurse to population ratio at 2013 levels. Considering that we even failed to maintain annual recruitment at 2013 levels and are just playing catch up, is there any wonder we are recruiting more but our nursing deficit is widening?
I will end with these words of caution; we can choose to bury our heads in the sand and play ostrich with bulk numbers. The reality is for as long as we are a member state of the World Health Organisation and continue to report our health data, we would only be fooling ourselves locally whilst exposing our naivety globally.
By Kwame Sarpong Asiedu
The post When the numbers confront the rhetoric in Ghana’s management of nurses appeared first on Ghana Business News.
]]>
According to Saidi Mdala, “bad luck is what results when bad things happen to you unprepared, or when you neglect to do what you have to do when you are supposed to do it.” This week I read of claims that medical personnel had neglected a patient leading to a loss of life. Whilst reading […]
The post How Ghana’s health system is making and breaking hearts appeared first on Ghana Business News.
]]>
 According to Saidi Mdala, “bad luck is what results when bad things happen to you unprepared, or when you neglect to do what you have to do when you are supposed to do it.”
According to Saidi Mdala, “bad luck is what results when bad things happen to you unprepared, or when you neglect to do what you have to do when you are supposed to do it.”
This week I read of claims that medical personnel had neglected a patient leading to a loss of life. Whilst reading that, I was also aware of a doctor who improvised to get an infant to a hospital where appropriate levels of urgent care could be provided. On his way back to his station, he also had to assist a mother in labour to deliver with the aided by a midwife.
The fact is, our health system always makes and breaks our hearts. It does because whilst a lot of good goes on, often too much goes wrong for the knights in shining amour to be seen in a positive light. There is a lot to be said about how we got here but I would rather on this occasion deal with what needs to change. For far too long, we as citizens have failed to accept that the healthcare, we receive is a direct consequence of our actions and inactions.
We have treated healthcare as though it is for the politicians and bureaucrats to decide what our needs are and how they are met. In doing so, we have allowed them to have a debate about health improvement using parameters that often have little bearing on our healthcare outcomes or quality of care. For as long as I have followed healthcare in Ghana, I have come to hear our debates focused mainly on inputs. For example, by how much infrastructure was enhanced under a particular government whether it is the building of new hospitals or the purchase of ambulances. In debating on inputs, we have failed to consider simple things like the prudence of spending decisions or whether value for money is a major consideration. On a few occasions, these debates shift to outputs in the sense of whether the infrastructure was delivered. Here too we never discuss the correlation between expenditure and results.
Few of us have sat to think and discuss how these inputs have helped to improve our healthcare by way of decreasing maternal mortality, infant mortality and ultimately improve life expectancy. We seem to forget that all the inputs and outputs are of no relevance if they cannot translate in real terms to tangible outcomes. We fail to ask whether at the end of it all we are living healthier and longer. Based often on our political lineage we wrongly assume that just by having infrastructure that we can visualize, we are better off from a quality of health viewpoint.
Unfortunately, this is extremely erroneous. Infrastructure can at best be described as tools and enablers that enhance the capability of a health system to deliver healthcare to society. Without the human resources in these facilities, the right attitudes and skills set, the infrastructure by themselves cannot change our health outcomes.
Clearly, from the positives and negatives I read about this week, there seems to be a range of attitudes in our health system. From the very motivated and determined who want to deliver quality care irrespective of obvious constraints and remain true to their professional oaths to those who at the least instance give up. To have the former is commendable but can we blame the latter? Can it be asserted that their behaviour is deliberate?
Several factors go into the motivation of health personnel. Important amongst them is a clearly defined role with a clear understanding of how the individual’s role fits into the wider goals of the health facility. Speaking to health professionals, I am aware that many have little idea of what the mission statement of their specific institution is, let alone know what the vision and goal are. How then can patients and or leaders in our health institutions expect the provision of optimal healthcare?
Another serious motivator is the provision of training and upskilling. This must not be limited to the leadership of these institutions but must be targeted at the frontline staff who are the face of care delivery. There are many aspects of health that rub shoulders with customer care and service yet it is rear to see such training provided to health professions before graduation or whilst on the job. It is strangely assumed that these soft skills come naturally. Should it then come to us as a surprise when it is claimed nurses on occasion can be rude and vile?
Another area that needs urgent addressing is empathy and understanding. This is because health facilities unlike recreational spaces are not visited by citizens because they want to but rather because they have to. In our country, many are known to avoid these places until they have virtually no choice. Thus, most patients arrive frustrated and anxious. In such a situation the caregiver must be adequately equipped to manage the patient in a manner that irrespective of potential health outcomes allay their fears. The skills required to achieve these professional qualities must be nurtured continually, a situation that does not pertain to many of our health facilities.
I have always insisted that no rational health professional will set out on a path to deliver poor healthcare. As was demonstrated by Dr Emmanuel Adipa-Adapoe last week the reverse is the case. On the contrary, many are to make ill health bearable. However, if they are left in a situation where the system is skewed in a way that they feel done to, the result is the negligence we sometimes hear of. That bad luck happens to us repeatedly indicates that our society has failed to plan and is often unprepared.
As citizens, we need to accept that just shouting about no bed syndrome, medical negligence or the absence of an ambulance to transport the sick child will not lead to changes that will prevent a recurrence. Changes will only happen when we begin to challenge public office holders on why all their claims on investment in health have not resulted in significant changes in health outcomes. Allowing them to have the usual banter around who has invested more is an exercise in futility. Ours is not bad luck but a situation in which citizens have neglected their responsibility to hold public office holders accountable for their failure to plan. By so doing we are bearing the brunt but sadly cheering our political stables on.
By Kwame Sarpong Asiedu
The post How Ghana’s health system is making and breaking hearts appeared first on Ghana Business News.
]]>
Roy T. Bennett in The Light in the Heart argues “Do not let the memories of your past limit the potential of your future. There are no limits to what you can achieve on your journey through life, except in your mind.” The 25th of September 2019 was World Pharmacists Day, celebrated this year with […]
The post Can we achieve safe and effective medicines for all? appeared first on Ghana Business News.
]]>
Roy T. Bennett in The Light in the Heart argues “Do not let the memories of your past limit the potential of your future. There are no limits to what you can achieve on your journey through life, except in your mind.” The 25th of September 2019 was World Pharmacists Day, celebrated this year with the theme “Safe and effective medicines for all.”
Since this day was designated by the International Pharmaceutical Federation (FIP) Council in Istanbul, Turkey in 2009. I have always used it as a day to reflect on the profession that has been the underpinning of my career since 1998. This year, I have felt rather conflicted in my reflection just because of the theme. I have because practising in a country that has been my home for most of my adult life and having a passion for the land in which my umbilical cord is buried, I see a serious disconnect.
The pharmaceutical definition of medicine is a drug used to diagnose, cure, treat, or prevent disease. Thus, for most humans’ medicines are part of their activities of daily living either by choice or as a result of a sudden or existing medical condition. In the country where I practice my profession, data indicates that less than 1% of medicines in the pharmaceutical supply chain are substandard, compared to 10%-30% in developing countries. Reliable data on the prevalence of substandard medicines in Ghana is hard to come by. However, the World Health Organisation estimates that 30% of all drugs on the Ghanaian market could be fake.
This situation is one that must be of grave concern to all especially those of us who profess to be “friends of the human race.” Apart from the risk of treatment failure with infectious diseases like malaria, it also impacts on chronic disease management like the control of blood pressure for hypertensives and glycaemic control in diabetes just to name a few. All of which could have serious consequences on the health of the patient or could even lead to mortality. On the part of prescribers, it can often mar their decision making in situations of treatment failure as they could be unsure whether the chosen treatment option is inappropriate.
The reality is, even with the trained eye, a pharmacist has no way to save gut feelings and reliance on the security of their pharmaceutical supply chain to identify substandard drugs. Many practitioners, as a result, rely on the recommendation of branded products where patients can afford as a means of circumventing the risks counterfeit medicines pose. This route, unfortunately, has also been rendered porous by unscrupulous individuals with a majority of these fake brands ending up in pharmaceutical markets of sub-Saharan Africa. According to Pfizer Global Security 2017, between 2004 and June 2016, counterfeit versions of 26 Pfizer medicines were detected in the legitimate supply chain of at least 60 countries, including the US, Canada and the UK. They further assert that about 38% of all branded Viagra on African markets are fake.
As a result of these breaches, many countries and trading blocks like the European Union have put protocols like the Falsified Medicines Directive (FMD) in place relying on digital technology to help in the fight against spurious medicines. On the contrary, many developing countries Ghana included have struggled to have a coordinated approach in this fight. Being the new frontier for organised crime and knowing that the loopholes are closing in the more lucrative Western pharmaceutical markets, the kingpins have turned their focus towards Africa. Leading to the European Union ranking Ghana as the sixth largest producer of fake drugs in the world in 2013. Since then a lot has taken place from a regulatory standpoint in Ghana at least to bring the situation under control. However, most of these efforts have been akin to a firefight as regulators like the Food and Drugs Authority and Pharmacy Council lack the resources to adequately police Ghana’s medicines supply chain.
To put real numbers to this problem, worldwide, it is estimated that the counterfeit drug market is worth up to US$200 billion. With WHO statistics indicating that 42% (US$84 billion) of detected substandard or falsified pharmaceuticals occurring in Africa. Using the law of averages, it can be inferred that each of the 54 African countries potential can be exposed to US$1.6 billion worth of substandard drugs annually. In 2018 Ghana’s total health spend as a percentage of GDP (US$65.19 billion) was 6.5%. Indicating that US$4.24 billion was spent on health in that year. Meaning, approximately 38% of our total health expenditure could potentially have been going towards this trade and the funding of criminal elements unknowingly. This is the true size of the problem and the source of my moral conflict.
We cannot sit and ignore this huge loss of limited state funds and hope that the situation would wish itself away. If the dumping of tramadol in West Africa and the warnings of the United Nations Office on Drugs and Crime (UNODC) are to be taken seriously, the situation is even going to get worse. The point is the penalties for engaging in the illicit trade of pharmaceuticals worldwide are not stiff enough. Apart from China where it is on record that some unscrupulous elements who engaged in this trade received hefty jail sentences with some even being executed, many culprits walk away with a fine or a nominal custodial sentence. In Ghana, though many drug peddlers are routinely arrested, few end up being jailed. More importantly, I am unaware of any major player locally who has been arrested, tried and jailed for offences in this area under the Public Health Act (Act 851). This situation has led to many criminals abandoning other forms of illicit activity and channelling their attention to this underworld niche.
Our society can never achieve “safe and effective medicines for all” if we are not prepared to confront this albatross. There is no likelihood of effective medicines if the safety of the pharmaceutical supply chain cannot be guaranteed. I believe many in my profession are aware of this but hapless as to what they can do individually or as a collective to lead the fight. Our laws in this area are robust enough but not enforced. The situation is made even more complicated by the peddling of medicines of all forms in almost every corner of the country. Education of the citizenry and public lectures have done little to empower the population. On the surface, it may look like a dead rubber but it needn’t be.
We must refuse to let the memories of our past or current predicament in this area prevent us from a vision of a future where this issue does not plague us all. Countries that have fashioned solutions to this problem have done so not just because of their wealth but because they have taken the problem seriously. We must begin to take it seriously too. Technology that democratises this area of health through the empowerment of the citizens exist and has been deployed in many countries. In 2018, the National Institution for Transforming India (NITI) announced that they would be partnering with US-based computer technology company Oracle13 to deploy blockchain technology to advance the traceability of pharmaceutical products. I count myself fortunate to have the originators of similar technology Sproxil and mPedigree as indigenes of the land of my birth but wonder why they have become unwelcome messiahs in their land.
I would conclude by asking if spending potentially 38% of our total health expenditure or 2.4% of our GDP on otherwise useless medicines does bot push as to rethink our national approach in this area, what would? The limits to solving this problem lie only in our minds and must be confronted.
By Kwame Sarpong Asiedu
The post Can we achieve safe and effective medicines for all? appeared first on Ghana Business News.
]]>
According to Brian Tracy, “all successful people men and women are big dreamers. They imagine what their future could be, ideal in every respect, and then they work every day toward their distant vision, that goal or purpose.” In his view, the size of your dream can be directly correlated with the extent of your […]
The post Framing a future path for health transparency in Ghana appeared first on Ghana Business News.
]]>
 According to Brian Tracy, “all successful people men and women are big dreamers. They imagine what their future could be, ideal in every respect, and then they work every day toward their distant vision, that goal or purpose.” In his view, the size of your dream can be directly correlated with the extent of your achievement. I have been pondering on this over the past week whilst trying to envisage how to refocus Ghana’s health agenda in this new world where even a decade is an extremely long time.
According to Brian Tracy, “all successful people men and women are big dreamers. They imagine what their future could be, ideal in every respect, and then they work every day toward their distant vision, that goal or purpose.” In his view, the size of your dream can be directly correlated with the extent of your achievement. I have been pondering on this over the past week whilst trying to envisage how to refocus Ghana’s health agenda in this new world where even a decade is an extremely long time.
Healthcare has in the last two decades evolved to a point where it is widely accepted that practitioners irrespective of how experienced or skilled are limited by their brainpower and that diagnosis, prognosis and quality of care all benefit from considerable decision support. These support systems rely on and are considerably underpinned by data. With our disease burden altering, data will become the new determinant of how our healthcare system progresses.
Sadly, our society has been late in coming to terms with this new reality. Starting from the individual citizen, very few of us are conversant with our basic health information. From our average blood pressure readings and any fluctuations thereof, our glycaemic status (sugar regulation) etc. to the information contained in our health records irrespective of whether it’s digital or manual. This lack of interest has led to a situation where health institutions and even the state have ignored the importance of this data to our overall wellbeing.
In the midst of all this, we have become saddled with the fact that over 60 per cent of our citizens do not access healthcare at a primary level annually. This situation though a public health concern has never become a priority. Apart from having an impact on the health and wellbeing of individuals and society at large, it minimises our ability to have accurate data on our primary healthcare. Thus, putting us at a disadvantage in the new charge in improving healthcare worldwide. Though we are all aware of the barriers that lead citizens not to access primary healthcare, the impact of this on our collective health must not be ignored. Even though the threat of heart attacks and strokes stirring us all in the face, personal motivation is not enough to ensure we surmount these barriers that hold us back.
It is therefore important that we explore other options. I will layout a few.
In the midst of all this, we have become saddled with the fact that over 60 per cent of our citizens do not access healthcare at a primary level annually.
In my opinion, the starting point should be the reinvigoration of the National Health Insurance Scheme. Laudable as this scheme is as a social intervention it has never achieved coverage of up to 50% of the population since its inception. Having achieved its highest coverage of 40% in 2015, usage of NHIS by citizens dropped to 36% in 2017 and had appreciated marginally to 36.3% by the first quarter of 2019.
Several reasons could be adduced for this. First, is the fact that most of the money the scheme receives is absorbed by recurrent expenditure leaving less than 10% to be invested. Meaning the usefulness of the scheme both to users and service providers is compromised. Another is the fact that many in the rural informal sector complain of lack of funds to pay premiums. Then there is the allegation of corruption amongst service providers and the high drug bill compounded by the relatively high cost of medicines for the management of chronic diseases.
Though all these are a reality, it cannot be disputed that in our setting, health insurance coverage is probably the essential driver to improving population health and decreasing mortality through the improvement of access and thereby ensuring early detection of chronic diseases. I believe therefore that there must be the utilization of unorthodox means never tried to increase the percentage of citizens it covers.
The first suggestion I would make is to change the current model of outpatient care with one that will be patient-led and rely on community outreach. This could be the first means of collecting patient data into a centralised digital system. This system must be designed with functionality to allow patients ownership to their health records. For me, this is where the first obstacle will be encountered. This is so because the age held misconception by many medics that any records generated in their premises are the property of the facility will have to be debunked. So, will the notion that health professionals know best and may be well placed to hold some information away from patients.
Once this is achieved, through active patient education, the motivation of patients to want to be part of a health database must be leveraged. Amongst the motivational options could be emphasising this new concept of democratisation of health record keeping and explaining how the liberalisation of ownership of their health records could lead to valuable data points for family members even unborn. It would also be important to debunk superstition and to explain clearly that many of the ailments that in the past were attributed to sorcery can be explained away through genetics and a better understanding of a family’s generational medical history.
Though all these are a reality, it cannot be disputed that in our setting, health insurance coverage is probably the essential driver to improving population health and decreasing mortality through the improvement of access and thereby ensuring early detection of chronic diseases.
Should patient and health professional buy in be achieved, the next obstacle I envisage would be the lack of interoperability amongst different health record systems. This could be circumvented in several different ways. The first will be the establishment of a national health centralised database that can be plugged into by different health providers in primary, secondary and tertiary care. Such a system though tried in countries like the United Kingdom affords itself to considerable cost and security concerns. Often, these costs would have to be recouped by the state through taxes; a situation that many objects to. In our setting, it also throws in the procurement angle and the potential for politically engineered state capture. Also, the central control and maintenance by the state have raised eyebrows in some settings. Should this option be discounted, the next will be to invite private providers to build these databases in partnership with health providers but ensure that these systems talk to each other and are not stan alone. Though from a business perspective, standalone systems will be in the best interest of service providers, it will significantly compromise the concept of continuity of care.
If these two obstacles are circumvented the other details around regulation and data protection can be ensured through already existing laws like the Data Protection Act. It will be important that regulators have an understanding of the intentions of system providers from the outset and have the capability to monitor their activity to ensure the integrity of patient identifiable data.
When this in place I see the following opportunities. A clear audit trail for all users of the National Health Insurance Scheme. A decrease in allegations of fraudulent claims made by service providers. A large database that will allow health trends and medicines procurement patterns to be monitored across the country. The potential for a generation with a patient owned comprehensive health record from the womb to the grave. A wealth of medical information that algorithms can research to improve the quality of care we receive and to improve healthcare access. But ultimately convert the nation’s health data into an enviable new fuel capable of driving the new General-Purpose Technology (GTP) that will define healthcare moving forward i.e. Artificial Intelligence (AI).
If we fail the consequences are grave and could convert us in a couple of decades into what historian Yuval Noah Harari has come to describe as the useless class. This is the aspect that scares me. To be successful at this we need to become a nation of dreamers for impossible when split up reads “I’m possible.”
By Kwame Sarpong Asiedu
The post Framing a future path for health transparency in Ghana appeared first on Ghana Business News.
]]>